Animal Care Services Vs Pasadena Humane Glendale

Health care professionals are among the most highly trained, driven and conscientious professionals. So, how is it that medical errors are a major public health problem and patients do not consistently receive evidence-based care?
Despite their education and desire to deliver the best care possible, health care professionals can be set up for mistakes by poorly designed medical devices, uncoordinated care processes and fragmented systems. Too often, these systems are designed in a way that do not account for how people actually interact with their work environment.
Human beings have limited attention spans. We perform worse when we are tired. We can only focus on one thing at time. We forget things. When systems ask us to go beyond these and other limits, failures can occur.
Urging clinicians to "try harder" or "be more careful" will not safeguard them against errors. Likewise, efforts to improve care solely through education often have minor and fleeting improvements, if any. To reduce or prevent such harms, the health care environment must be designed with human limitations and abilities in mind.
This is the focus of human factors, a scientific discipline that aims to help people do their best work, improve resilience and overall system performance, and minimize errors. Human factors-based solutions make it "easy to do things right and hard to do things wrong." When errors do occur, they are less likely to lead to patient harm.
Applications of Human Factors in Health Care
In health care, human factors specialists seek to improve people-system interactions for everyone involved – health care professionals, patients and family members. Their work can be focused on enhancing the safety and usability of a single product – such as a medical device – or on improving an entire care delivery process or organizational structure (e.g. leadership, supply-chain management, etc.). These specialists seek to understand the myriad factors that affect performance of the system — the physical environment; tasks, tools and technologies involved; and the organizational conditions in which the work occurs — and then redesign systems to improve patient safety and team performance.
These methods can be used to:
- minimize clinician error
- improve clinician performance
- increase delivery of evidence-based medicine
- enhance patient- and family-centeredness of care
- improve patient-provider communication
- reduce inefficiencies and non-value adding tasks
- reduce burnout and improve clinicians' job satisfaction
While human factors approaches have been used for decades in complex, high-risk fields such as aviation and nuclear power, their introduction to health care was limited until the Institute of Medicine's 1999 landmark report, "To Err is Human: Building a Safer Health Care System." Even today, these approaches are not widely adopted, and more work is needed to integrate human factors methods and tools into health care improvement work.
Human Factors in Action: Examples from the Field
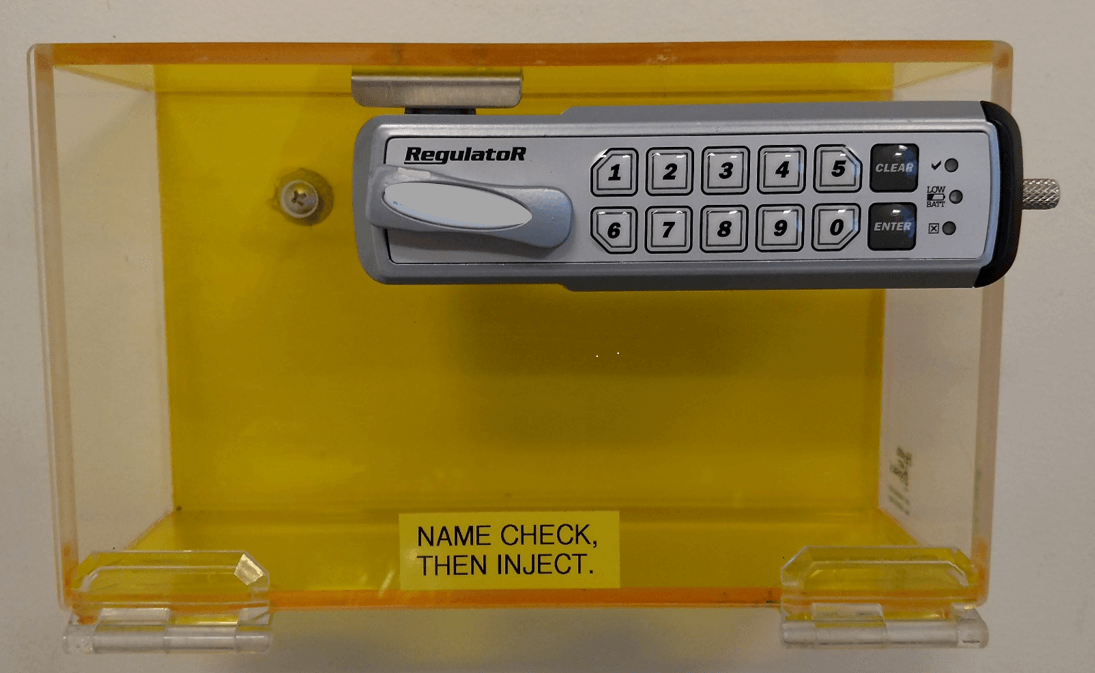
Safe Medication Storage
Multidose insulin pens are required to be placed in patient-specific containers in a medication room, per both Johns Hopkins and Joint Commission requirements. However, patient needs, physician requests, phone calls and other interruptions often caused nurses to put the pens in their pockets and make a mental note to return them later. This practice led to medication errors.
Working with a human factors engineer, a unit-based safety team devised, installed and evaluated clear plastic lockboxes in each patient's room to hold an insulin pen.
Learn more
Improving Safety of Cardiac Surgery
Human factors engineers, clinicians, outcomes researchers, psychologists and sociologists sought to proactively identify safety risks in cardiac surgery using a multi-method approach, including observations of 22 surgeries at five well-respected hospitals. Their holistic review uncovered 58 different types of hazards — anything in the work system that has the potential to cause an error — related to flawed devices, suboptimal physical layout design, processes and organizational structures. Hazards included disorganized medication carts that might lead a clinician to select the wrong drug, a surgeon who was introduced to a new cautery gun in the middle of a procedure, and purchasing practices that did not consider the downstream safety impacts of their decisions. Many of the team's recommendations were adopted by the five hospitals, resulting in improvements in areas such as infection prevention and safety of care transitions.
See related journal article.
Preventing Infusion Pump Errors
There were instances in which the tubing from an infusion pump would come into contact with the pump's touch screen, leading to accidental changes in the rate of infusion. Working with a human factors engineer, the team added a Plexiglas, see-through guard that enables clinicians to move the tubing without accidentally changing the pump's settings.
"Human factors and ergonomics must play a more prominent role in health care if we want to increase the pace in improving patient safety."
- Gurses AP, Ozok AA, Pronovost PJ. "Time to accelerate integration of human factors and ergonomics in patient safety." BMJ Qual Saf 2012; 21:347-351.
Animal Care Services Vs Pasadena Humane Glendale
Source: https://www.hopkinsmedicine.org/armstrong_institute/centers/human_factors_engineering/human_factors_in_health_care.html
0 Response to "Animal Care Services Vs Pasadena Humane Glendale"
Post a Comment